This new national audit report comes at a time when there is major interest in the use of non-invasive respiratory support, including NIV and CPAP therapies.
Acute NIV can be a lifesaving treatment for specific patients. The emergence of COVID-19 has certainly increased attention around its use. It is important to note, though, that this audit does not include any data from patients with COVID-19, as the audit period was 1 February – 31 March 2019, long before the emergence of the disease in the UK. This was the largest to date with 3502 patient submissions, compared with 2693 patient submissions in the previous audit in 2013.
The last national audit in 2013 highlighted a worsening trend in outcomes, with high mortality rates and significant institutional variation. The British Thoracic Society then successfully proposed a national study via the National Confidential Enquiry on Patient Outcomes and Death (NCEPOD). NCEPOD methodology includes a detailed review of case notes, providing new insights into many of the issues raised by earlier BTS audits.
NCEPOD’s report in 2017 highlighted wide variation in both the organisation of acute NIV services and the clinical care provided. It did show areas of good practice, but all too often found evidence of treatment delay, suboptimal treatment delivery and deficiencies in the organisation of services. Key concerns included insufficient levels of nursing staffing, NIV treatment delivery in inappropriate locations, and inadequate treatment monitoring. Overall, the quality of care was rated as ‘less than good’ in 80% of cases reviewed.
NCEPOD made key recommendations for service improvement and these were reinforced by the BTS Quality Standards for acute NIV (2018), which provided a series of quality statements as markers of high quality, cost-effective and evidence-based patient care. The BTS also published a Quality Improvement toolkit for NIV in the same year. There have been a significant number of publications on this technique since the last BTS national audit in 2013 which we hope would have made a positive impact on NIV services.
How did you select the questions you included in the audit?When developing audit questions it is important to draw on nationally agreed standards of care. We used the following documents:
• BTS/ICS Guideline for the ventilatory management of acute hypercapnic respiratory failure (2016)
• BTS Quality Standards for Acute Non-Invasive Ventilation (2018)
• National Confidential Enquiry into Patient Outcome and Death (NCEPOD) Report ‘Inspiring Change: A review of the quality of care provided to patients received acute non-invasive ventilation’ (2017).
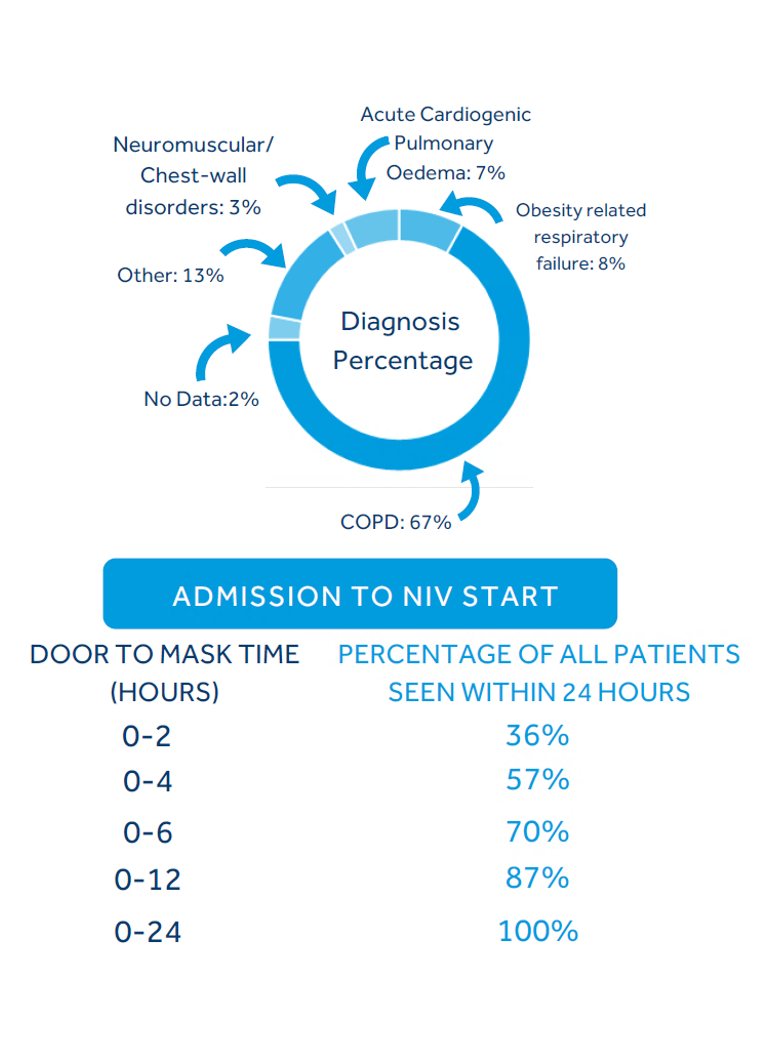
What does the new audit tell us about the patients who are receiving NIV?Identifying the right patients for a treatment is a very important aspect of care. The audit showed that an increased proportion of patients treated with NIV had COPD, the indication with the strongest evidence. We also saw a decreased proportion of patients who were treated with NIV despite no clearly documented indication. This is encouraging news, suggesting improved patient selection in line with the evidence base for NIV.
However, it is not just about selecting the right patients, it is also important to get NIV started promptly. We saw in this audit that 50% of patients treated with NIV started their treatment within 60 minutes of the result of the blood gas test defining the need for NIV. This is the first time that we have assessed treatment timing in this way. Compared to earlier audits, clinicians reported that a smaller proportion of patients had been subject to treatment delay in the most recent audit.
Have these improvements against standards provided direct benefit to patients?Yes, we are seeing some improvement in outcomes. The data shows that acute NIV was successful in resolving respiratory acidaemia for 76% of patients treated, in comparison to 69% in the last audit.
The better news is that overall inpatient mortality was 26% and has reduced from 34% in 2013. This is the first time that mortality has improved since the first BTS audit in 2010.
The BTS audit also highlighted what is happening at an organisational level. That is true. We know that only 74% of organisations reported that they have sufficient capacity to deliver the routine acute NIV service, meaning that more than a quarter of hospitals continue to lack sufficient capacity.
Whilst most services had a medical lead, only a minority had time dedicated in their jobs to provide this leadership.
Importantly, only 52% of organisations had a nursing lead and 34% had a physiotherapy lead for their acute NIV service. We know that the delivery of a successful acute NIV service is a truly multidisciplinary effort and it is disappointing that this is not reflected in trust leadership roles. This is an area that we have prioritised as a key national improvement target.
There are still improvements to be made. How can outcomes for patients improve further?The audit report includes the following national improvement objectives:
1. Improve patient selection for NIV, evidenced by reducing the proportion of patients who start NIV in the absence of a clearly documented evidence-based indication (current audit = 13%: target <10%)
2. Increase the proportion of patients who start NIV within 60 minutes of the blood gas that defines its need (current 50%: target >60%)
3. Increase the proportion of NIV services that have a named nursing lead and/or physiotherapy lead with time allocated to provide service leadership (current 69%: target >90%)
The current audit is hugely encouraging, showing multiple areas of clear improvement in the last few years. The national improvement targets serve as a framework for further improvement. However, there is still much to be done and it remains the case that there are substantial institutional variation in outcome. Some organisations still lack the infrastructure to provide effective NIV services. For example, survival was 11% higher for patients treated in an NIV-designated respiratory ward area compared to those treated in an area that had not been designated to deliver NIV. If all organisations who are commissioned to provide acute NIV ensured that they had the necessary service structure to provide this treatment, then I believe that variation in outcome would reduce and patient outcomes would improve further.
How do the findings of the 2019 audit relate to the recent circumstances of the COVID-19 pandemic?I feel that this is a hugely important topic at present. The recent circumstances around COVID-19 have really highlighted the key position of respiratory services in the provision of acute care. Nurse, Allied Health Professionals, and doctors with expertise in acute NIV provided an invaluable resource for the Critical Care and ward-based responses.
It is too early to make firm conclusions, but initial reports show that non-invasive techniques, such as CPAP and NIV, have had a life-saving impact. My personal experience at Royal Papworth Hospital was strongly supportive of CPAP therapy for severe hypoxaemic respiratory failure due to COVID-19. It also strongly affirmed the strengths and benefits of close collaboration between Respiratory and Critical Care colleagues.
There is no doubt that acute NIV services have shown some improvements in the last few years, but it is also the case that there has been insufficient national and organisational focus on this vital part of acute care. I hope that the improving outcomes within the 2019 audit and positive signal from the COVID response will act as a stimulus for a greater investment in acute NIV services.
This is an important time for sharing best practice and collaborating with others, particularly when respiratory services are being recast. How can help?It certainly is important that we encourage collaboration as it is always useful to hear from other teams about how their services are set up and managed. We have seen some really fantastic abstracts submitted to BTS Summer and Winter Meetings over recent years and it would be good to see more good practice shared through Respiratory Futures.
If you have a story of innovation or best practice in NIV which you would like to share with the respiratory community, email us at contact@RespiratoryFutures.org